Celiac disease is an autoimmune disorder in which the ingestion of gluten— a protein found in wheat, barley, and rye— triggers an immune response that damages the small intestine. This damage impairs nutrient absorption and can lead to a variety of health issues. Understanding celiac disease, recognizing its symptoms, and knowing how to manage it through a gluten-free lifestyle are crucial for those affected by this condition. This blog provides a comprehensive overview of celiac disease, including its symptoms, diagnostic procedures, and tips for living gluten-free.
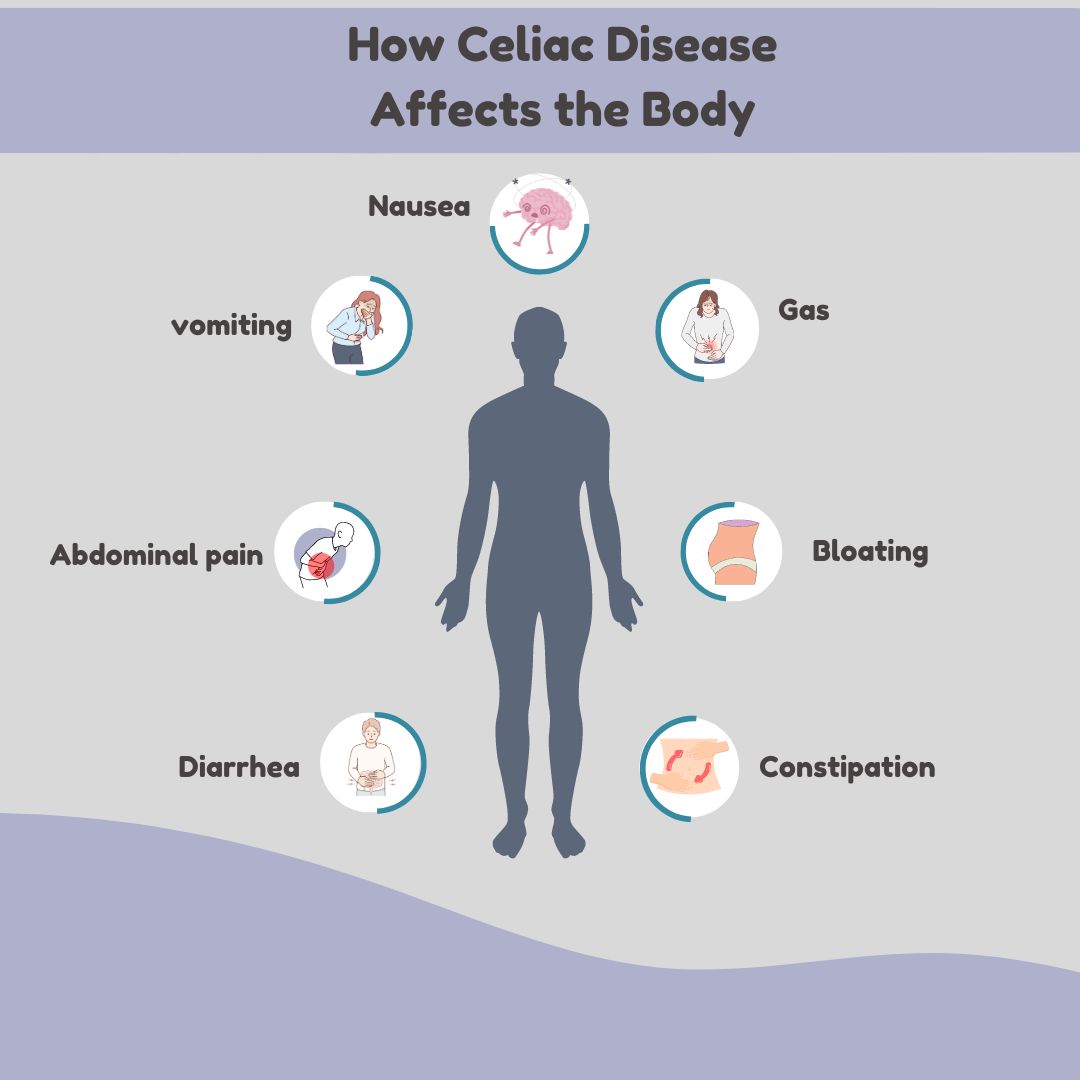
Digestive Symptoms:
-
Abdominal Pain: Cramping or pain in the stomach area.
-
Bloating and Gas: Excessive gas production and abdominal swelling.
-
Diarrhea: Frequent, loose, and watery stools.
-
Constipation: Difficulty passing stools or infrequent bowel movements.
-
Nausea and Vomiting: Feelings of queasiness and throwing up.
Non-Digestive Symptoms:
-
Fatigue: Persistent tiredness or lack of energy.
-
Weight Loss: Unintentional weight loss despite normal eating habits.
-
Anemia: Low red blood cell count, often due to iron or vitamin deficiencies.
-
Skin Rash: Dermatitis herpetiformis, an itchy, blistering skin rash.
-
Bone and Joint Pain: Aches or discomfort in bones and joints.
-
Symptoms in Children:
-
Delayed Growth: Slower growth rate compared to peers.
-
Short Stature: Shorter height for age.
-
Irritability: Increased moodiness or fussiness.
-
Failure to Thrive: Poor weight gain and growth.
Symptoms in Adults:
-
Infertility: Difficulty conceiving or recurrent miscarriages.
-
Osteoporosis: Weakening of bones due to malabsorption of calcium and vitamin D.
-
Neurological Symptoms: Numbness, tingling in the extremities, or peripheral neuropathy.
Diagnosing Celiac Disease
Diagnosing celiac disease involves a combination of clinical evaluation, blood tests, and sometimes a biopsy. The diagnostic process typically includes:
-
Medical History and Physical Examination:
-
Assessment: A healthcare provider will review the patient's symptoms, medical history, and perform a physical examination to identify signs consistent with celiac disease.
-
Blood Tests:
-
Serological Tests: Blood tests can detect specific antibodies associated with celiac disease, including:
-
Anti-Tissue Transglutaminase (tTG) Antibodies: Elevated levels suggest an immune response to gluten.
-
Anti-Endomysial Antibodies (EMA): Presence of these antibodies further supports the diagnosis.
-
Deamidated Gliadin Peptide (DGP) Antibodies: Useful in diagnosing celiac disease in cases with ambiguous results.
-
Genetic Testing:
-
HLA Typing: Testing for specific genetic markers (HLA-DQ2 and HLA-DQ8) can help assess the risk of developing celiac disease. While the presence of these markers alone does not confirm celiac disease, their absence makes it unlikely.
-
Endoscopy and Biopsy:
-
Procedure: An upper endoscopy involves inserting a thin, flexible tube with a camera through the mouth to examine the small intestine. During this procedure, a biopsy is taken to evaluate damage to the villi.
-
Evaluation: Histological examination of the biopsy sample confirms the diagnosis by identifying villous atrophy and inflammation.
Living Gluten-Free: Managing Celiac Disease
The primary treatment for celiac disease is adhering to a strict, lifelong gluten-free diet. Here are some tips for living gluten-free:
-
Understanding Gluten-Free Foods:
-
Safe Foods: Fresh fruits, vegetables, lean meats, fish, dairy products, and gluten-free grains (e.g., rice, quinoa, and millet) are naturally gluten-free.
-
Avoiding Gluten: Wheat, barley, rye, and products containing these grains must be avoided. Common sources include bread, pasta, cereals, and baked goods.
-
Reading Labels:
-
Product Labels: Always check food labels for gluten-containing ingredients. Look for products labeled “gluten-free” to ensure they meet safety standards.
-
Hidden Gluten: Be aware of hidden sources of gluten, such as sauces, soups, and processed foods that may contain gluten as a thickener or additive.
-
Avoiding Cross-Contamination:
-
Food Preparation: Use separate utensils, cookware, and surfaces for gluten-free food preparation to avoid cross-contact with gluten-containing products.
-
Eating Out: Communicate with restaurant staff about gluten-free options and ensure that proper procedures are followed to prevent cross-contamination.
-
Nutritional Considerations:
-
Balanced Diet: Ensure a balanced diet by including a variety of gluten-free grains, fruits, vegetables, and protein sources to meet nutritional needs.
-
Supplements: Consider supplements for nutrients that may be lacking in a gluten-free diet, such as iron, calcium, vitamin D, and B vitamins.
-
Support and Education:
-
Support Groups: Joining celiac disease support groups or online communities can provide valuable information and emotional support.
-
Continuous Learning: Stay informed about celiac disease and advancements in gluten-free food options and products.
Conclusion
Celiac disease is a serious autoimmune disorder that requires careful management through a strict gluten-free diet. Recognizing the symptoms, undergoing appropriate diagnostic tests, and adhering to a gluten-free lifestyle are essential for managing the condition and maintaining overall health. With proper education, vigilance, and support, individuals with celiac disease can lead healthy and fulfilling lives while avoiding the adverse effects of gluten consumption. If you suspect you have celiac disease or need guidance on managing the condition, the team at Digestive and Liver Disease Consultants, P.A. is here to provide expert care and support.