End-stage liver Disease (ESLD) can feel overwhelming, but understanding the condition, its management, and where to seek help can make a big difference in improving quality of life. ESLD is the final phase of chronic liver disease, when the liver's ability to function effectively has been severely compromised. Whether you’re seeking guidance for yourself or a loved one, this guide will break down the essentials of ESLD in simple terms and outline how Digestive & Liver Disease Consultants, P.A., can help.
What is End-Stage Liver Disease?
The liver plays a vital role in your body, performing tasks like detoxifying harmful substances, producing bile for digestion, and storing essential nutrients. When the liver is damaged over time due to chronic conditions like cirrhosis, hepatitis, or fatty liver disease, its ability to perform these functions diminishes.
ESLD occurs when the liver has suffered severe, irreversible damage. It’s often associated with symptoms like:
- Fatigue
- Jaundice (yellowing of the skin and eyes)
- Abdominal swelling (ascites)
- Confusion or memory issues (hepatic encephalopathy)
- Easy bruising or bleeding
If you or a loved one is experiencing these symptoms, it’s essential to seek medical attention promptly.
What Causes ESLD?
The most common causes of ESLD include:
Chronic Alcohol Use: Long-term alcohol abuse can lead to cirrhosis, a major risk factor for ESLD.
Chronic Hepatitis B or C: These infections can cause ongoing liver inflammation, leading to scarring and liver failure.
Non-Alcoholic Fatty Liver Disease (NAFLD): Often linked to obesity, diabetes, and high cholesterol, NAFLD can progress to severe liver damage.
Autoimmune Liver Diseases: Conditions like autoimmune hepatitis or primary biliary cholangitis attack the liver, causing long-term harm.
Diagnosis of ESLD
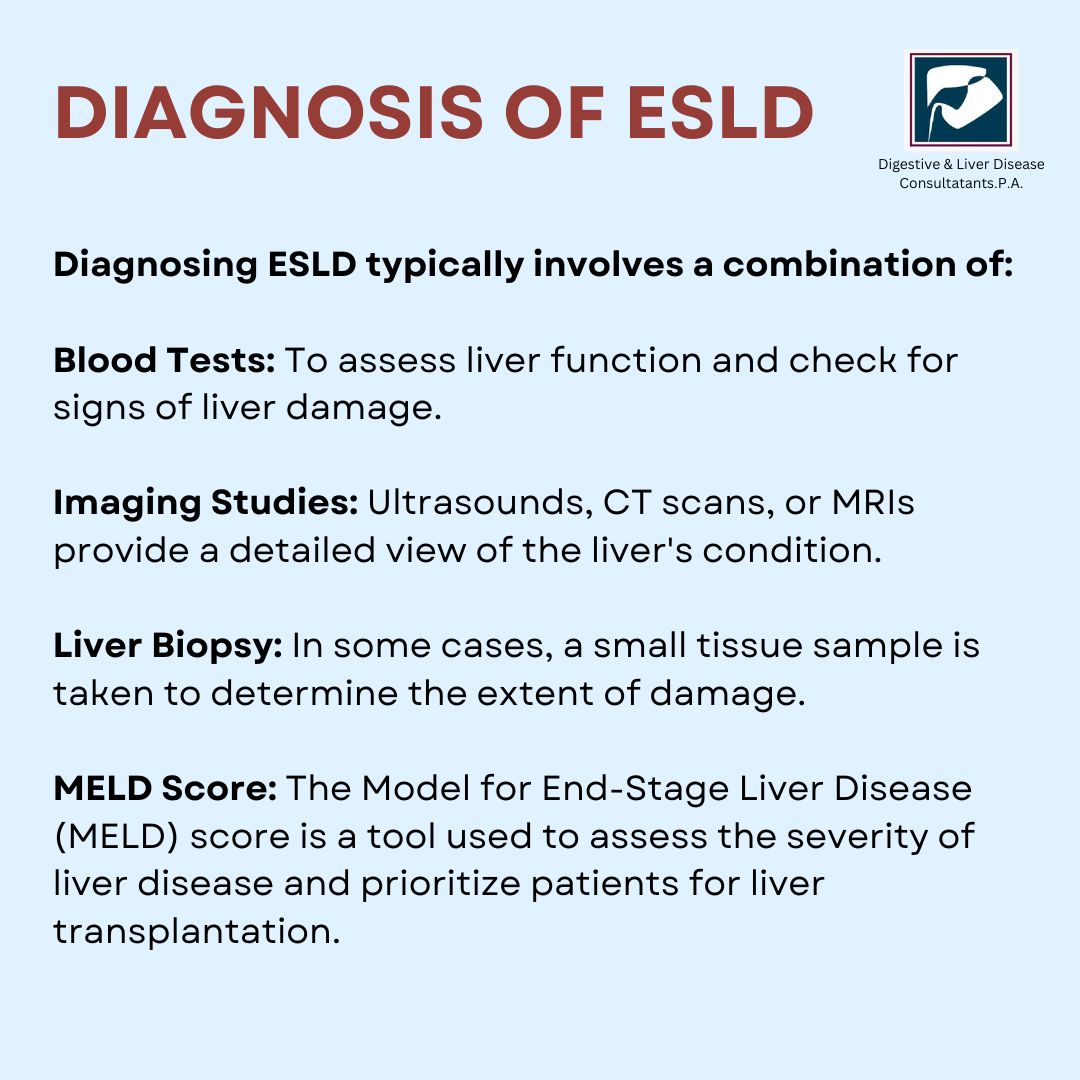
Diagnosing ESLD typically involves a combination of:
Blood Tests: To assess liver function and check for signs of liver damage.
Imaging Studies: Ultrasounds, CT scans, or MRIs provide a detailed view of the liver's condition.
Liver Biopsy: In some cases, a small tissue sample is taken to determine the extent of damage.
MELD Score: The Model for End-Stage Liver Disease (MELD) score is a tool used to assess the severity of liver disease and prioritize patients for liver transplantation.
Managing End-Stage Liver Disease
While ESLD is a serious condition, there are ways to manage symptoms, prevent complications, and improve quality of life. Here’s how:
1. Lifestyle Adjustments
Making lifestyle changes is often the first step in managing ESLD:
- Avoid Alcohol: Even small amounts can worsen liver damage.
- Adopt a Healthy Diet: Focus on low-sodium, high-protein foods to reduce fluid retention and maintain muscle mass.
- Stay Active: Gentle exercises, like walking, can help maintain physical strength.
2. Medications
Your doctor may prescribe medications to:
Manage symptoms like itching or pain.
Reduce fluid buildup in the abdomen.
Treat complications, such as infections or encephalopathy.
3. Monitoring and Regular Checkups
Frequent medical checkups help monitor disease progression and manage potential complications like bleeding or kidney problems.
4. Liver Transplantation
For many with ESLD, a liver transplant is the best option. A healthy liver from a donor replaces the damaged one, restoring normal function. However, not everyone is a candidate for transplantation, and careful evaluation is needed.
Why Choose Digestive & Liver Disease Consultants, P.A.?
At Digestive & Liver Disease Consultants, P.A., we specialize in diagnosing and treating a wide range of liver conditions, including ESLD. Our board-certified gastroenterologists and hepatologists bring years of experience and a patient-centred approach to care. We understand the emotional and physical challenges of living with ESLD, and we are here to support you every step of the way.
Our services include:
- Comprehensive diagnostic evaluations, including advanced imaging and liver biopsies.
- Customized treatment plans tailored to your needs.
- Access to the latest medications and therapies.
- Ongoing monitoring and management of symptoms and complications.
- Coordination with transplant centers for eligible patients.
We aim to help you achieve the best possible outcomes while improving your quality of life.
Conclusion
End-Stage Liver Disease is a serious condition, but with the right care and support, it’s possible to manage symptoms and maintain a better quality of life. If you or a loved one is living with ESLD, don’t wait to seek help.
At Digestive & Liver Disease Consultants, P.A., we’re here to guide you every step of the way. Whether you’re managing symptoms or considering a liver transplant, our team is ready to provide the expert care you need.