Diabetes and liver disease often go hand in hand. When high blood sugar and insulin resistance combine with liver stress, complications can develop that affect overall health. Managing liver disease in diabetes is essential to prevent further damage and improve quality of life.
Understanding the Link Between Diabetes and Liver Function
People with diabetes are at higher risk of developing liver problems, including non-alcoholic fatty liver disease (NAFLD in diabetic patients). Insulin resistance, high blood sugar, and chronic inflammation can contribute to fat accumulation in the liver, liver inflammation, and fibrosis.
Uncontrolled blood sugar can worsen liver function, while liver damage can, in turn, affect glucose metabolism. This creates a cycle that can increase the risk of liver complications in diabetes if left unchecked.
Common Liver Issues in Diabetic Patients
Fatty Liver Disease
Fatty liver is the most common liver condition in people with diabetes. It occurs when excess fat accumulates in liver cells. While early stages may be silent, over time it can progress to inflammation, scarring, and even cirrhosis.
Liver Inflammation and Fibrosis
Chronic liver inflammation in diabetic patients increases the risk of fibrosis. Early detection through regular liver monitoring in diabetes is critical to prevent permanent damage.
Liver Complications Diabetes Can Trigger
Unchecked diabetes increases the risk of
- Liver cirrhosis
- Liver failure
- Increased susceptibility to infections
- Impaired detoxification
Understanding these risks highlights why diabetes liver management must be proactive.
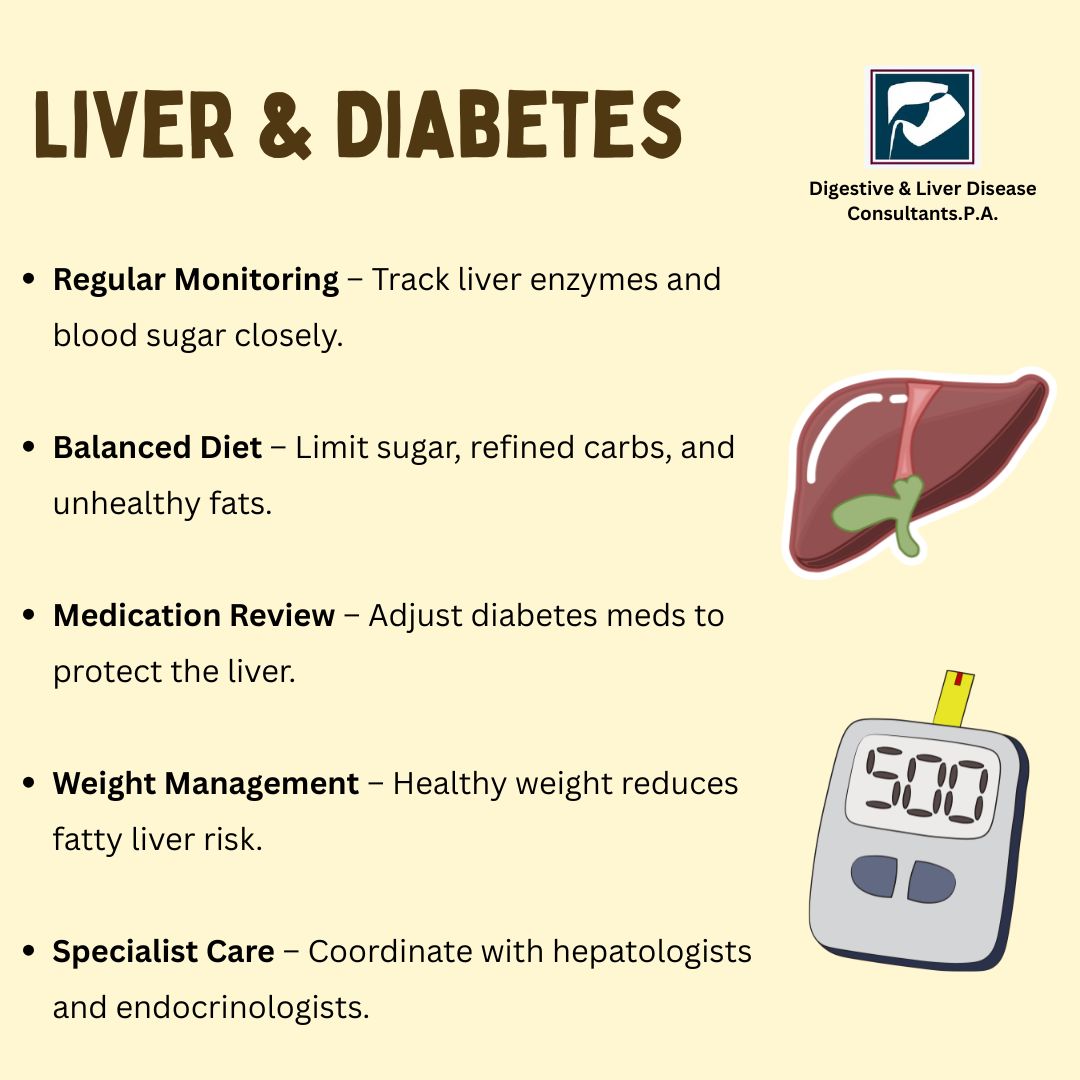
Key Strategies for Managing Liver Disease in Diabetes
1. Control Blood Sugar and Insulin Levels
Blood sugar and liver health are closely linked. Maintaining stable glucose levels reduces fat accumulation in the liver and lowers the risk of inflammation. Steps include
- Regular monitoring of blood sugar
- Following prescribed diabetes medications
- Tracking HbA1c levels to assess long-term control
Effective glucose management is foundational for diabetic liver care.
2. Adopt a Liver Friendly Diet Diabetes
A diabetic liver diet focuses on nutrient-rich foods that reduce fat in the liver and support metabolism. Key recommendations include
- Whole grains, legumes, and vegetables
- Lean protein sources like fish, chicken, and tofu
- Healthy fats from nuts, seeds, and olive oil
- Limited sugar, refined carbs, and fried foods
- Avoiding alcohol
These dietary choices play a central role in managing fatty liver diabetes and improving overall metabolic health.
3. Maintain a Healthy Weight
Weight management helps reduce fat in the liver. Even modest weight loss of 5–10