Irritable Bowel Syndrome is one of those conditions that can turn your everyday routine upside down. One day you feel fine, and the next day your gut decides to do its own thing. If you live with IBS, you already know how unpredictable it can be. But here is the thing: IBS symptoms do not just appear out of thin air. There are specific triggers that set the stage. Once you recognize them, you can manage your symptoms with a lot more confidence and control.
What IBS Really Is
IBS is a functional digestive disorder. That means the structure of your gut is normal, but how it moves, reacts, and communicates with your brain is not always smooth. Symptoms can include abdominal pain, bloating, constipation, diarrhea, or a mix of both. IBS does not damage the intestines and it does not lead to cancer, but it absolutely affects your daily life.
Understanding your triggers is the first real step toward relief.
1. Food Triggers
Food is the biggest culprit for most people with IBS. The problem is that triggers vary from person to person. Still, some foods commonly cause trouble.
High FODMAP foods
These are foods that contain fermentable carbohydrates that pull water into your gut and create gas. Examples include onions, garlic, apples, honey, beans, cauliflower, wheat products, and dairy. A low FODMAP diet has helped many people identify their biggest sensitivities.
Greasy or fried foods
These slow down digestion and push your gut to work harder. Many people notice cramps or diarrhea soon after eating fried chicken, pizza, burgers, or creamy sauces.
Caffeine and alcohol
Both can stimulate the colon. Coffee, energy drinks, beer, and wine may worsen urgency or diarrhea.
Artificial sweeteners
Sugar substitutes like sorbitol, mannitol, and sucralose can cause bloating and gas.
Large meals
Eating too much at once puts pressure on the digestive system and increases the chance of discomfort.
What this really means is that your journal is your best friend. Tracking what you eat and how your gut responds is one of the most effective ways to find your patterns.
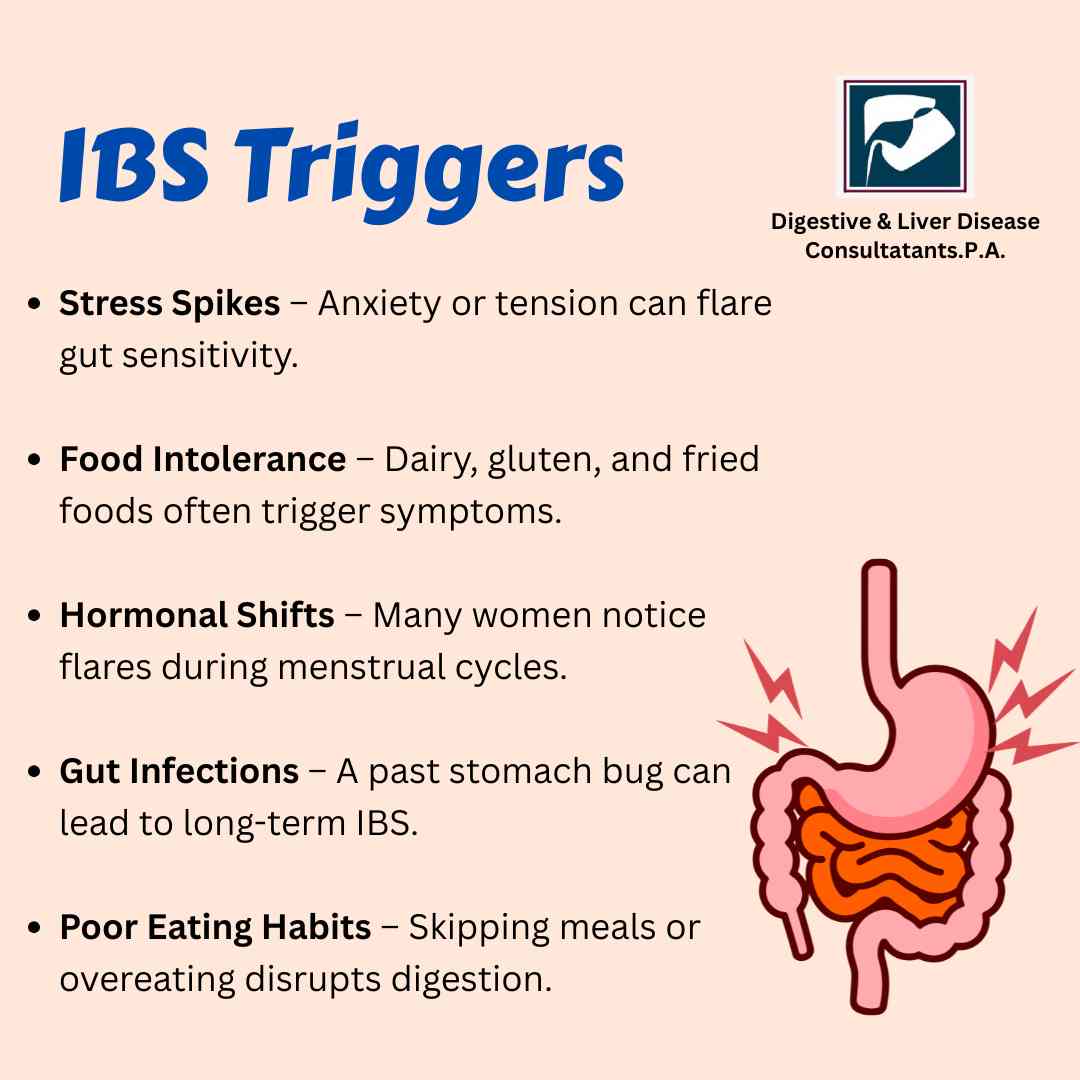
2. Stress and Emotional Triggers
Your brain and gut are always talking to each other. When stress rises, your gut reacts. Emotional triggers like anxiety, overthinking, lack of sleep, and high pressure at work or home can cause major flares.
Here is the thing. Stress does not cause IBS, but it absolutely fuels it. When your stress level spikes, your colon becomes extra sensitive and moves either too fast or too slow.
Some helpful habits include breathing exercises, short walks, mindful eating, journaling, and regular sleep. Even fifteen minutes of quiet time a day can calm your symptoms.
3. Hormonal Changes
Hormones play a huge role in IBS, especially for women. Many women report more IBS symptoms around their menstrual cycle.
Hormonal shifts can change gut motility and sensitivity. If this sounds familiar, tracking your cycle alongside symptoms may reveal a pattern.
4. Gut Sensitivity
People with IBS often have a more sensitive digestive system. Something that might not affect others can hit you harder. Even normal amounts of gas can cause pain if your gut nerves are overly reactive.
This sensitivity can also be connected to past infections, inflammation, or changes in the gut microbiome.
5. Medications
Some medicines can irritate the digestive tract or affect bowel movements. Common ones include:
- Antibiotics
- Antidepressants
- Pain medications like NSAIDs
- Magnesium based supplements
- Iron supplements
If you noticed your symptoms starting after a medication change, make sure to tell your doctor.
6. Gut Infections and Food Poisoning
A sudden stomach infection or food poisoning can leave long lasting effects on the gut. This is called post infectious IBS. Even after the infection clears, the gut nerves stay sensitive and digestion becomes irregular.
7. Lack of Fiber or Too Much Fiber
Fiber helps regulate bowel movements, but the wrong kind of fiber or the wrong amount can make symptoms worse.
- Too much insoluble fiber like raw vegetables, bran, or tough greens can trigger bloating and pain.
- Too little soluble fiber like oats, bananas, or sweet potatoes can lead to constipation.
The key is balance. Most people with IBS do best with gentle, soluble fiber.
8. Dehydration
When you are dehydrated, your intestines struggle to move waste smoothly. This leads to constipation, hard stools, or incomplete bowel movements. Drinking enough water throughout the day helps keep digestion steady.
9. Physical Inactivity
Your gut loves movement. When your body stays inactive for too long, your digestion slows down. Even a simple daily walk can help ease constipation, reduce bloating, and improve overall comfort.
Why Identifying Triggers Matters?
IBS is different for everyone. What bothers one person might not affect another at all. That is why managing IBS is not about avoiding everything, but about understanding what affects you personally.
Once you identify your triggers, you get:
- Better symptom control
- More predictable digestive comfort
- Fewer emergency bathroom moments
- Less stress around food
- Better quality of life overall
Working with a digestive specialist can make this process much easier and faster.
How Digestive & Liver Disease Consultants, P.A. Helps IBS Patients?
Digestive & Liver Disease Consultants, P.A. is known for providing advanced, patient focused digestive care in the US. Their team of experienced gastroenterologists understands how complex IBS can be. They combine detailed evaluation, modern diagnostic tools, and personalized treatment plans to help patients manage IBS with confidence.
Patients receive support through:
- Comprehensive digestive assessments
- Low FODMAP diet guidance
- Medication and treatment plans tailored to IBS type
- Gut health and microbiome focused care
- Lifestyle and stress management strategies
- Long term follow up
Their approach focuses on improving your quality of life, not just treating symptoms. Whether your IBS is mild, moderate, or severe, the team provides the care you need with compassion and expertise.
When to See a Doctor?
If your symptoms are frequent, severe, or affecting your daily life, it is time to get help. You should see a gastroenterologist if you notice:
- Unexplained weight loss
- Severe abdominal pain
- Rectal bleeding
- Symptoms that wake you up at night
- Persistent diarrhea or constipation
- A sudden change in bowel habits
- Food fear or meal related anxiety
IBS is manageable, but you should never ignore new or worsening symptoms.
Conclusion
IBS can be challenging, but it is not unbeatable. Most triggers are manageable once you understand how your body responds. Pay attention to your food habits, stress levels, sleep routine, hydration, and activity. Small changes make a big difference.
And if you ever feel stuck or unsure, you do not have to handle it alone. The digestive specialists at Digestive & Liver Disease Consultants, P.A. are here to help you find clarity, relief, and a long term plan that works for your lifestyle.
If you are suffering from IBS symptoms or need expert guidance, schedule an appointment with Digestive & Liver Disease Consultants, P.A. today. Your gut health deserves the right care.