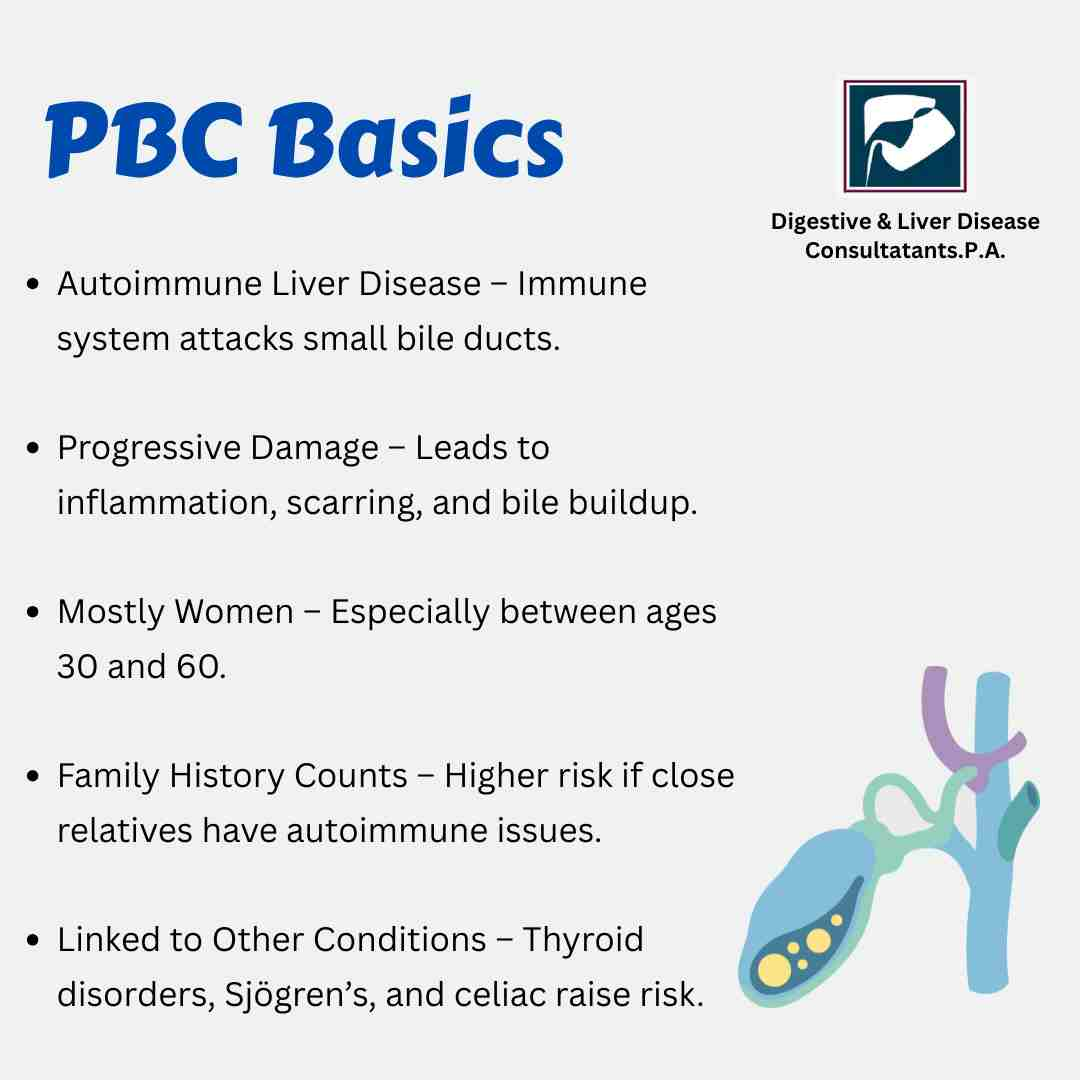
Primary Biliary Cholangitis, or PBC, is one of those conditions people often hear about only after a routine blood test shows unusual liver markers. It’s an autoimmune liver disease, which means the body’s immune system mistakenly targets its own healthy cells. In PBC, these attacks happen in the small bile ducts inside the liver. When these ducts get damaged, bile can’t flow out the way it should. It starts building up, and that buildup slowly injures liver tissue.
What this really means is that early diagnosis matters more than most people realize. With the right care, people with PBC can live full and healthy lives. The key is understanding what it is, how it shows up, and who is most at risk.
How PBC Starts and Progresses
Here’s the thing. PBC doesn’t happen overnight. It moves through stages, each based on how much damage the liver has experienced. In early stages, the bile ducts are inflamed but still present. As the condition progresses, the ducts shrink, bile backs up, and liver cells start to scar.
Doctors often find PBC accidentally. A patient may go for a routine health exam, and their liver enzymes, especially alkaline phosphatase, show elevated levels. Further tests reveal antimitochondrial antibodies, or AMA, which are present in most people with this disease.
Once confirmed, treatment usually focuses on protecting the liver, reducing inflammation, and keeping bile flowing. The earlier this starts, the better the long-term outcome.
Common Symptoms of PBC
PBC can be sneaky. Many people with early PBC feel completely fine. But when symptoms appear, they tend to follow a common pattern.
Fatigue is usually the first noticeable sign. It feels different from normal tiredness and doesn’t improve with rest.
Another big one is itching. It tends to be more intense at night and can show up long before any liver complications appear.
Dry eyes and dry mouth are also common because PBC sometimes overlaps with other autoimmune conditions.
As the disease progresses, symptoms may expand to include:
- Skin darkening
- Pain in the upper right abdomen
- Yellowing of the skin or eyes
- Bone or joint pain
- Swelling in legs or ankles
- High cholesterol
- Digestive issues due to poor fat digestion
Not everyone experiences the same symptoms. Some feel only mild discomfort, while others deal with several issues at once.
Who Is at Risk for Primary Biliary Cholangitis?
Now let’s look at the risk factors. The tricky part is that researchers still don’t know exactly what triggers PBC. It has nothing to do with alcohol. It’s not caused by unhealthy habits or lifestyle choices. It seems to be a mix of genetics, environment, and autoimmunity.
Here are the groups who are more likely to develop PBC:
Middle aged women
About 9 out of 10 people with PBC are women, most between ages 30 and 65. Hormones may play a role, but the exact reason is still unclear.
People with a family history
If a close relative has PBC or another autoimmune disease, the chances increase. That doesn’t guarantee someone will get it, but it does raise the risk.
Those with other autoimmune conditions
PBC often goes hand in hand with conditions like thyroid disease, rheumatoid arthritis, Sjogren syndrome, celiac disease, and autoimmune hepatitis.
Environmental exposures
Some studies suggest a possible link with smoking, chronic infections, or exposure to certain chemicals, but none of these are proven causes.
Genetic predisposition
Certain gene variations may make some individuals more vulnerable. This doesn’t mean the disease is inherited directly. It simply means genes may influence the body’s immune response.
If you’re in one or more of these groups, it doesn’t mean you will develop PBC. It simply means awareness and routine testing are especially important.
How PBC Is Diagnosed
Diagnosis usually starts with bloodwork, especially tests that check liver enzymes. A consistently high alkaline phosphatase level is a major indicator. The presence of AMA antibodies strongly supports a PBC diagnosis.
Doctors may also order imaging tests like ultrasound or MRI to rule out other causes of bile duct problems. In some cases, a liver biopsy provides more clarity.
At Digestive and Liver Disease Consultants, P.A., our specialists use a combination of advanced diagnostic tools and clinical expertise to identify PBC early. The goal is simple. Understand what your liver is telling you and act before irreversible damage sets in.
Treatment Options for PBC
Here’s where early care really pays off. While there’s no cure yet, treatment can slow or even stop the disease’s progression.
The main medicine used is Ursodeoxycholic acid, or UDCA. It improves bile flow and reduces liver inflammation. Many people respond very well to it, especially when treatment starts early.
For those who don’t respond to UDCA alone, there are newer medications that target inflammation and bile acid buildup.
Symptom-based care is also part of treatment. For example:
- Medicines for itching
- Supplements for bone health
- Vitamin support if nutrient absorption is affected
- Lifestyle changes like limiting fried foods or managing cholesterol
Regular follow up tests help doctors track the liver’s health and adjust treatment as needed.
Living With PBC
Living with PBC takes a combination of medical care and self awareness. Most people continue their daily routines with little change, especially when the condition is caught early.
Staying active, maintaining a balanced diet, avoiding smoking, and keeping a healthy weight all help protect the liver. Stress management also helps because autoimmune flare ups often worsen when stress levels stay high.
What matters most is consistent care from a liver specialist who understands the nuances of autoimmune conditions.
How Digestive and Liver Disease Consultants, P.A. Can Help?
DLDC has deep experience managing autoimmune liver conditions like PBC. Our board certified gastroenterologists and hepatologists use evidence based care to evaluate, diagnose, and treat patients with chronic liver diseases.
We offer advanced diagnostic tools, personalized treatment plans, and long term follow up to help you stay ahead of liver related complications. Whether you’re dealing with unexplained fatigue, unusual blood test results, or questions about your liver health, our team provides the guidance you need.
When to See a Doctor
If you’ve been experiencing unexplained itching, persistent fatigue, or abnormal liver enzyme levels, it’s worth getting checked. Early detection dramatically changes the course of PBC.
If you have a family history of autoimmune diseases, regular monitoring is a smart move even if you feel perfectly healthy.
And if you’ve already been diagnosed, partnering with a specialist ensures you’re receiving the most effective and up to date care.
Final Thoughts
PBC can seem intimidating, but knowledge changes everything. The more you understand how it develops and who is at risk, the easier it becomes to take control of your health. With the right care and consistent monitoring, most people with PBC live long, healthy lives.
If you’re experiencing symptoms or have concerns about your liver health, the specialists at Digestive and Liver Disease Consultants, P.A. are here to help. Reach out for expert evaluation and personalized treatment that supports your long term well being.