Frequently Asked Questions
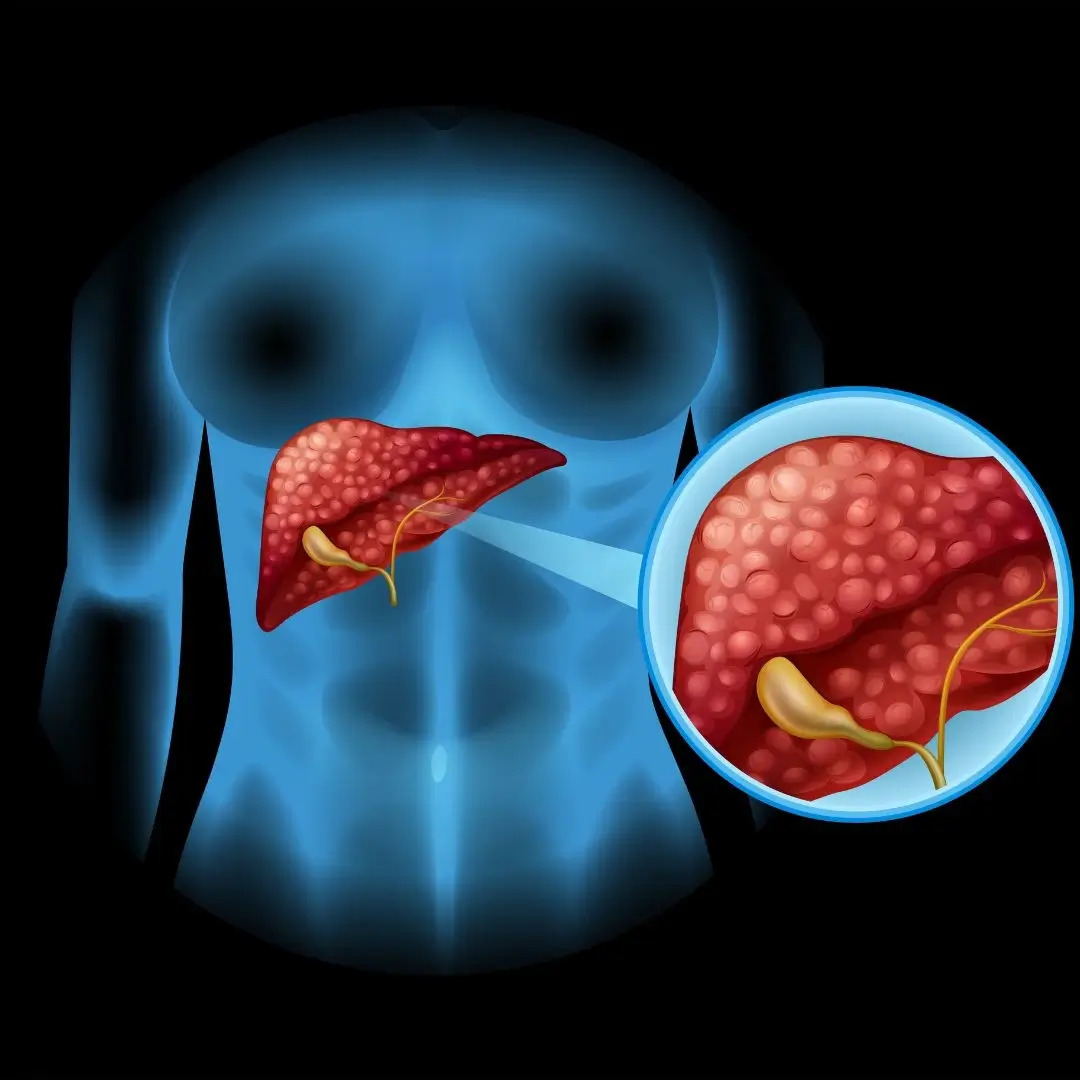
Fatty liver disease is a condition where excess fat builds up in the liver cells, affecting liver function.
Common causes include obesity, diabetes, high cholesterol, alcohol use, and metabolic syndrome.
Most patients have no symptoms, but some may experience fatigue, abdominal discomfort, or weight loss.
Diagnosis is done by blood tests, imaging like ultrasound or FibroScan, and sometimes liver biopsy.
Yes, with lifestyle changes and treatment, fatty liver disease can often be reversed or improved.
Treatment includes weight loss, healthy diet, exercise, managing diabetes and cholesterol, and avoiding alcohol.
There are no specific FDA-approved medications, but some drugs can help manage related conditions.
Losing 5-10% of body weight can significantly improve liver fat and inflammation.
Yes, untreated fatty liver disease can progress to fibrosis, cirrhosis, and liver failure.
Alcohol should generally be avoided as it worsens liver damage.
Healthy diet, regular exercise, weight management, and controlling diabetes are key.
Possible complications include liver inflammation, fibrosis, cirrhosis, and increased risk of cardiovascular disease.
Regular monitoring every 6-12 months is recommended based on severity.
Yes, nonalcoholic fatty liver disease can affect children, especially those with obesity.
Yes, diabetes is a major risk factor and often coexists with fatty liver disease.