Frequently Asked Questions
Hepatic encephalopathy is a decline in brain function due to severe liver disease, where toxins build up and affect the brain.
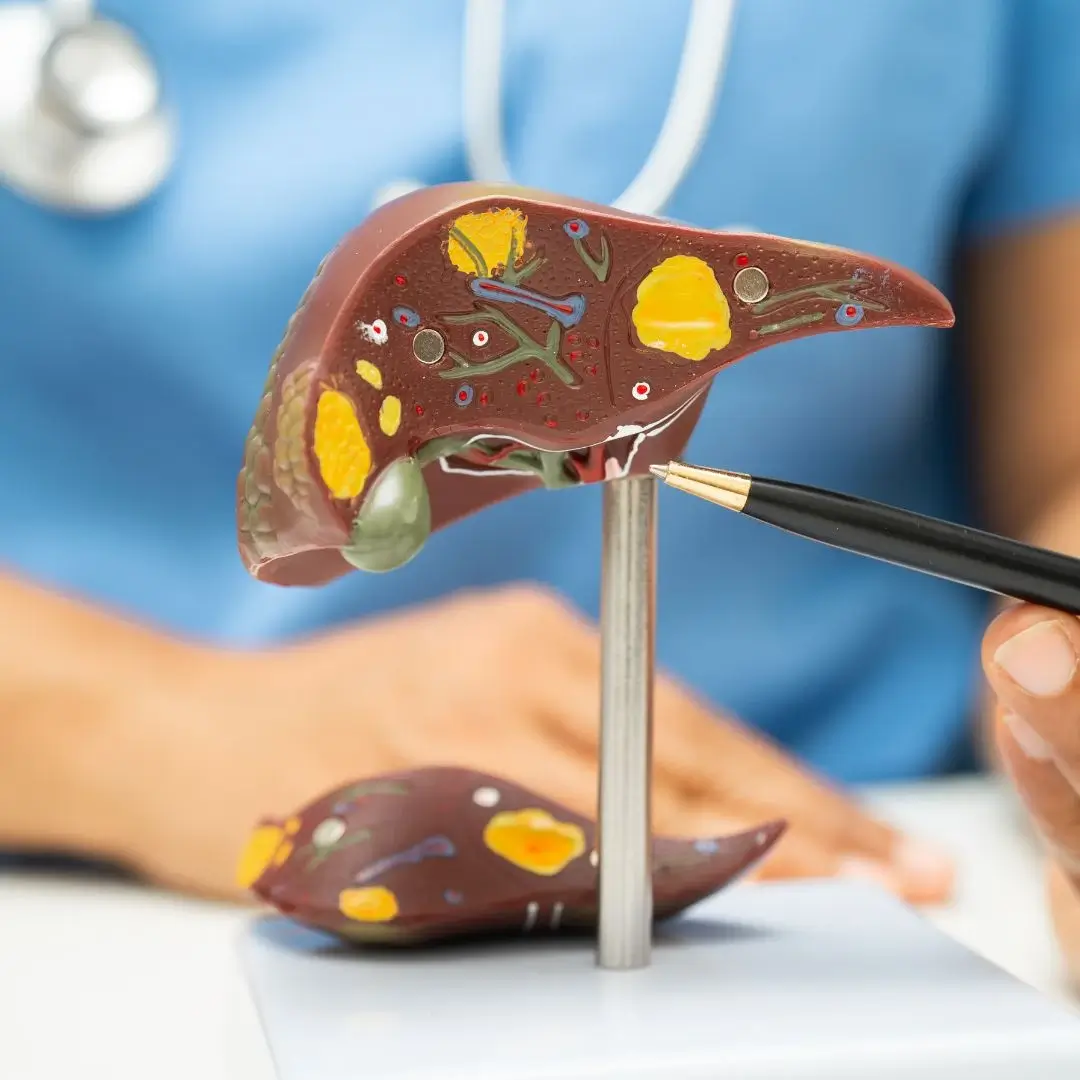
It is primarily caused by advanced liver disease or cirrhosis, which impairs the liver’s ability to filter toxins like ammonia.
Symptoms include confusion, mood changes, difficulty concentrating, altered sleep patterns, slurred speech, and in severe cases, coma.
Diagnosis involves clinical evaluation, blood ammonia tests, liver function tests, and ruling out other causes of confusion.
Treatment includes lactulose to remove ammonia and antibiotics like rifaximin to reduce toxin-producing gut bacteria.
Yes, early stages can be reversed with treatment and lifestyle changes, but recurrent or severe episodes may cause permanent damage.
A low-protein diet may be recommended initially, followed by a balanced protein intake with plant-based or dairy proteins.
Yes, it can recur, especially if liver disease is not well controlled. Long-term management is essential to prevent relapse.
Common triggers include infections, gastrointestinal bleeding, dehydration, constipation, and electrolyte imbalances.
Seek emergency care if there's sudden confusion, disorientation, loss of consciousness, or signs of liver failure.
Complications include recurrent hospitalizations, memory loss, reduced quality of life, and increased risk of coma.
Not always. Mild cases can be managed at home with medications, but moderate to severe cases often require hospital care.
It is most common in people with cirrhosis, but in rare cases, it can occur in patients with acute liver failure or portal-systemic shunting.
Yes, through alcohol avoidance, proper liver disease management, avoiding triggers, and regular follow-ups with a liver specialist.
Yes, in eligible patients with end-stage liver disease, liver transplantation can cure hepatic encephalopathy by restoring liver function.