Digestive discomfort is common, but not all gut problems are the same. Two conditions that are often confused are IBD and IBS. While their names sound similar, they are very different in cause, severity, and treatment. Misunderstanding these conditions can delay proper care and worsen symptoms.
Understanding Gut Disorders
The digestive system is complex, and chronic digestive conditions can affect daily life in many ways. Some conditions involve inflammation and tissue damage, while others affect how the gut functions without causing visible injury.
This distinction is the key to understanding inflammatory bowel disease vs irritable bowel syndrome.
What Is IBS?
Irritable bowel syndrome is a functional gut disorder. This means the digestive tract looks normal on tests, but it does not function properly.
IBS affects how the intestines move and respond to stimuli like food and stress. It does not cause inflammation, ulcers, or permanent damage.
Common IBS Symptoms
IBS symptoms tend to fluctuate and may worsen during stress or dietary changes.
Typical IBS symptoms include:
- Abdominal pain or cramping
- Bloating and gas
- Diarrhea, constipation, or alternating both
- Mucus in stool
- Relief of pain after bowel movements
IBS symptoms can be uncomfortable and frustrating, but they are not life threatening.
What Is IBD?
Inflammatory bowel disease is a serious medical condition involving chronic inflammation of the digestive tract. The two main types are Crohn’s disease and ulcerative colitis.
Unlike IBS, IBD causes visible inflammation, ulcers, and tissue damage that can be seen on imaging and endoscopy.
Common IBD Symptoms
IBD symptoms are often more severe and persistent.
They may include:
- Chronic diarrhea
- Abdominal pain
- Blood in stools
- Unintended weight loss
- Fatigue
- Fever
- Anemia
IBD is a progressive condition and requires long term medical management.
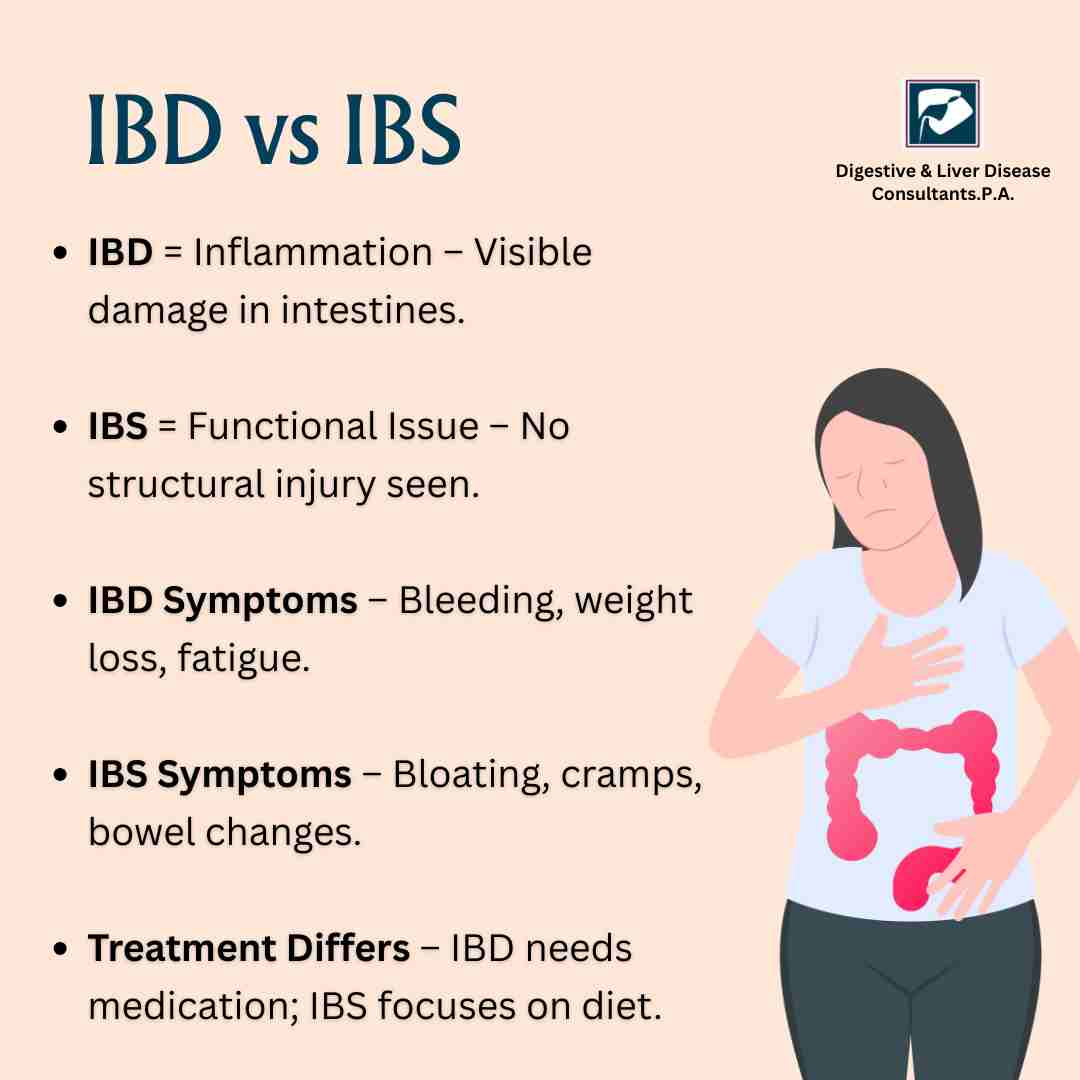
Difference Between IBD and IBS
Understanding the difference between IBD and IBS is critical for proper diagnosis and treatment.
Nature of the Condition
- IBS is a functional disorder
- IBD is an inflammatory disease
Physical Damage
- IBS does not damage the intestines
- IBD causes inflammation, ulcers, and scarring
Diagnostic Tests
- IBS tests often appear normal
- IBD shows abnormalities on blood tests, stool tests, imaging, and endoscopy
Risk of Complications
- IBS does not increase cancer risk
- IBD increases the risk of colon cancer and other complications
This gut disorders comparison highlights why the two conditions should never be treated the same way.
Causes and Triggers
IBS Triggers
IBS is often triggered by:
- Stress and anxiety
- Certain foods
- Hormonal changes
- Gut sensitivity
The exact cause is unknown, but nerve signaling between the brain and gut plays a major role.
IBD Causes
IBD is linked to:
- Immune system dysfunction
- Genetic factors
- Environmental triggers
The immune system mistakenly attacks the digestive tract, leading to chronic inflammation.
Diagnosis: Why Medical Evaluation Matters
Many people self diagnose IBS and ignore symptoms that may actually point to IBD.
IBS is diagnosed based on symptoms and exclusion of other conditions.
IBD requires:
- Blood tests for inflammation
- Stool tests
- Colonoscopy or endoscopy
- Imaging studies
Without proper testing, chronic digestive conditions like IBD may go untreated for years.
Treatment Approaches
IBS Management
IBS treatment focuses on symptom control.
This may include:
- Dietary changes
- Stress management
- Fiber or antispasmodic medications
- Probiotics in selected cases
IBS management is personalized and often lifestyle driven.
IBD Treatment
IBD treatment aims to reduce inflammation and prevent complications.
It may involve:
- Anti inflammatory medications
- Immune suppressing drugs
- Biologic therapies
- Nutritional support
- Surgery in advanced cases
IBD always requires specialist care.
Can IBS Turn Into IBD?
No. IBS does not turn into IBD. However, early IBD can sometimes be mistaken for IBS because initial symptoms overlap.
This is why persistent or worsening symptoms should never be ignored.
Warning Signs That Point Toward IBD
Seek immediate medical attention if you experience:
- Blood in stools
- Persistent diarrhea lasting weeks
- Nighttime bowel movements
- Weight loss without effort
- Fever or severe fatigue
These are not typical IBS symptoms and require evaluation for inflammatory bowel disease.
Living With Chronic Digestive Conditions
Both IBS and IBD can impact quality of life, but the approach to management is different.
IBS requires patience, lifestyle adjustments, and symptom tracking.
IBD requires medical supervision, regular monitoring, and adherence to treatment to prevent flare ups and complications.
Knowing which condition you have empowers you to manage it correctly.
Conclusion
The debate of IBD vs IBS is not just about terminology. It is about understanding the seriousness of symptoms and choosing the right care. The difference between IBD and IBS lies in inflammation, intestinal damage, and long term risks.
While IBS is uncomfortable, IBD is a chronic inflammatory disease that demands early diagnosis and expert treatment. Confusing the two can delay care and lead to complications.
If digestive symptoms persist, worsen, or interfere with daily life, professional evaluation is essential.
If you are experiencing ongoing digestive symptoms and want clarity on whether it is IBS or IBD, consult the experts at Digestive & Liver Disease Consultants, P. A. Our best gastroenterologists specialize in diagnosing and managing complex gut disorders with personalized, evidence based care.
Book your appointment today and take control of your digestive health with confidence.